Healthlocker for the NHS
Support patients and improve care teams’ workflow
Duration: 5 months
Teammates: 1 service designer, 1 visual designer, 1 PM, 1 front-end engineer
Process: service user and carer interviews, doctor interviews, competitive analysis, personas, patient record system training, prototype testing.
The Maudsley Hospital, the largest mental health training institution in the UK, sponsored the creation of a web app helping the communication between mental health service users and their care team. This project aimed to identify how technology could promote self-management and challenge what a personal health record should be. I was hired as a UX designer to envisage the new flow and address issues raised by a previous version of the app.
Deliverables
A responsive web application that provides a series of tools, resources and contacts to support self-management
Integration with patient record system (ePJS)
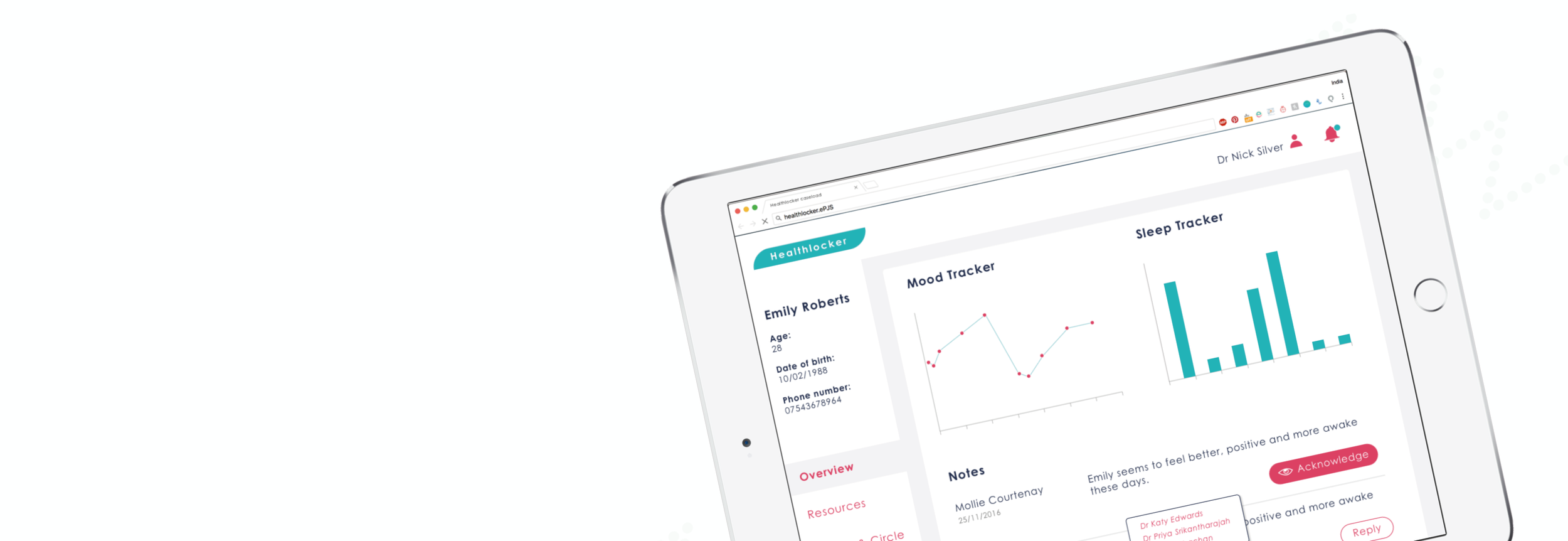
A platform with a clinician entry point and interface specific to the care team providing an overview of the patient care
Discovery
Analysing user needs
With cutback to health services, technology has the potential to relieve overstretched care teams and support service users. Back in 2016, there was a gap in the mental health management market and tools like Pacifica (now called Sanvello) were in their early days.
User research involving more than 400 clinicians and service users had already done before my involvement. Our team workshops helped us analyse the data gathered, highlight recurring themes, prioritise our user groups and understand their needs.
South London and Maudley clinian
“Workflow simplification is paramount for healthcare providers. If you’re unable to integrate with existing processes and systems, you’re creating additional work. Doctors and nurses don’t want to be logging out and logging in. Nobody wants to duplicate information, even hitting Alt + Tab — I don’t want to do that, it’s not seamless enough. Electronic Health Record is king in the modern world of healthcare workflow.”

Deconstructing myHealthlocker
MyHealthlocker, the previous version of the project launched in 2012 but failed to retain service users and their care team.
We unveiled the following the problems:
Repeated and lost information due to the app and the patient recording system not talking to each other
Clinician didn’t log in as they perceive it to be an additional effort
Non-responsive website, difficult to access on mobile on the go
Limited self-management help outside of appointments
Friction in the sign up and login journey leading people to abandon once they have an issue like a forgotten password
Out of date design with obsolete content
Building for service users (patients)
Through our research, we established personas and a general vision for the new Healthlocker.
We wanted to shift the balance from service users receiving care towards supported self management, especially while waiting for their next appointment. They should have access useful information and advice to help them cope. They could invite their carer to connect and share information with each other. The app could also contribute to their existing clinical record and allow access to anonymous data for academic researchers if consent was given.
Service user
“It would be good to be able to add new strategies and tailor to yourself.”
Carer
“Keeping a record of the changes - all the information is there, the daily stuff. Absolutely magic.”

Mental health service user posting about their user needs

Service user sharing their tips for other struggling with their mental health

Service user's weekly schedule to build empathy and understand how the app could fit in their daily life

Building for clinicians
The success of our project depended greatly on simplifying the care team workflow. Therefore, integration with their current patient record system (ePJS) was at the forefront of our development partner’s work. We wanted to support clinicians by providing information that’s easy to digest in the short amount of time they have to prepare for an appointment.
The app needed to improve communication between service users, clinicians and carers. It also required to meet national directives around the digital transformation of care and be a pioneer in the development of PHR. We built this product in an open source, modular way that would allow for future integrations.
Explorations
Prototyping the journey
We discovered clinicians were uneasy about opening a communication line for the service users to reach out. Even though studies showed patients would not contact their care provider unless an emergency occurred, perception of increased workload would greatly influence doctor’s use of Healthlocker. Furthermore, it raised safeguarding issues for communication outside of working hours and without controlled hospital environment with secure digital systems protecting patient data.
We pivoted our communication strategy and priorities to focus on the following:
Healthlocker is about giving service users self-management tools between appointments.
Providing a community supporting individuals with personal stories and tips as well as inviting carers
Mood tracker concepts
One of our priorities was to design a tool that would enable service users to access parts of their health records and contribute to it. The mood tracker allowed users to keep track of their own mental else between appointment. It also gave a quick overview to clinicians, whose time is a very limited resource.

Concept for the care team view of a service user's info

Receiving feedback from an NHS doctor on a paper prototype

Patient record system interface from a training day




Iterating
Challenge highlight: security vs usability tread-off
As we were dealing with confidential medical information, our stakeholders were keen on adding security measures. They suggested service users would require to log onto the app with a password and a 4 number code.
However, the previous version of the app saw an abandonment rate partly due to people who forgot their credentials. To limit the weight on IT, we considered a self-serve journey for password and passcode recovery relying solely on the account’s email address.
After several discussion on the security vs usability tread-offs, we finally decided to implement one password instead of two.
Further thoughts
Healthlocker later evolve into Maia, a patient engagement portal with the following features:
Add more info to patient record file
Health tracking data compatible with wearables and other third-party trackers
Data collection forms for medical researchers
Send messages to clinicians with attachments
Connect with friends, family and carers
Developing an app for the NHS can be a challenge. Any project targeting by patients and dealing with medical data requires a lot of scrutiny to make sure it is conform to guidelines. Furthermore, electronic patient record systems are complicated legacy systems with interfaces that are difficult to navigate for both patients and care teams, wasting time and precious knowledge.
Despite these complex problems, working in the health sector is an opportunity to create solutions that deeply impact the life of patients. For this reason, I decided to go back to university in 2018 to study the more theoretical and academic aspects of designing for healthcare through a Master in Human-Computer Interaction at UCL.
As a designer, I strongly believe creating digital tools can assist professionals in their craft so they can focus on what they’re best at. However, there’s so much an app can do when the resources and funding in mental health services are limited. This case study only focuses on the early phase of Healthlocker and I am pleased to see this tool has greatly evolved since 2016.